Radio-Induced Maxillary Angiosarcoma: About a Case
Abstract
Introduction
Angiosarcoma is a rare malignant tumour from fast-evolving and aggressive vascular endothelial cells that accounts for 1% of all sarcomas. The sinus location of angiosarcoma is exceptional. The clinical polymorphism of this tumour may cause a delay in diagnosis. Risk factors are not always understood. However, a history of radiation therapy for locoregional cancer and/or lymphedema is most commonly found. The prognosis remains bleak with an overall five-year survival of 35 to 40%.
Objectives
The authors discuss the diagnostic, therapeutic and prognostic modalities and difficulties of this tumour. Observation: The authors report a case of maxillary sinus angiosarcoma confirmed by radio-induced secondary CD34 immunohistological staining in a 40-year-old man having a history of hemangioendothelioma treated with conservative endoscopic surgery and adjuvant radiotherapy 15 months earlier.
Discussion
This lesion is rare in the ENT sphere and may be confused with a benign tumor in its early stages. Only histological examination with immunohistochemistry can confirm the diagnosis (factor VIII, CD34 and CD31 antigens). Treatment consists of a wide resection followed by radiotherapy, hence the need for early diagnosis in the metastatic phase, first-line treatments include doxorubicin or paclitaxel weekly.
Conclusion
Radio-induced angiosarcoma is a rare malignant tumour, it occurs in patients who have received conservative treatment and radiation therapy for nasosinusitis cancers. Angiosarcomas of the nasal passages remain a diagnostic and therapeutic challenge due to their local and general aggressiveness.
Author Contributions
Copyright © 2025 Mohamed Hachemi, et al
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
No funding was received to assist with the preparation of this manuscript.
Citation:
Introduction
Angiosarcomas are aggressive malignant tumours from mesenchymal cells that account for 1% of all sarcomas 1, with more than 50 subtypes of histopathological variants 2, and a high frequency in the neck and head region in patients with no medical history 3. The nasal sinus angiosarcoma is a rare manifestation of paranasal and nasal sinuses, with a low incidence of about 0.1% 4, may be without any associated risk factors or radio-induced in patients who have received conservative treatment for cancer, including conservative surgery and adjuvant radiation therapy 4. The diagnosis of nasal angiosarcoma remains a diagnostic challenge, due to its low incidence and mild symptoms in the initial stage 3. The diagnosis of angiosarcoma can be clinically evoked by the presence of nasal obstruction, swelling of the face with or without epistaxis, radiologically by the presence of a tumor that takes contrast to CT and signs of aggression of surrounding structures, Howeve the definitive diagnosis is based on histological study, systematically associated with immunohistochemistry 5. Angiosarcomas occur frequently in any region of the head and neck. Although cases of nasal angiosarcoma are rare in the medical literature, their incidence has increased over the past decade 6. Surgery remains the primary treatment if possible, although some cases have been treated with radiation therapy with or without chemotherapy 7.
Observation
Patient aged 40 years without any surgical medical history who consults at our level in 2022 for a right epistaxis of average abundance with nasal obstruction and an induration next to the maxillary sinus right to palpation. Endoscopy revealed a reddish polypoid mass filling the right nasal cavity without palpable cervical adenopathies, CT returned in favor of an expansive tissue process of the right maxillary sinus, extended to the soft parts and the homolateral nasal cavity. The complete resection of the mass was performed by endonasal surgery (endoscopic maxilectomy). The histological examination found hemangioendothelioma without signs of malignancy with infiltrated margins, external complementary radiotherapy was indicated (50 Gy, 2Gy per day for 5 days a week on the maxillary sinus), a radiological check (MRI) 4 months later does not find any residual tumor. After an absence of 15 months, the patient revisits for resumption of symptomatology with right epistaxis of great abundance requiring 2 globular units, a reddish mass protruding from the nasal vestibule, lysing the bony palate with extension towards the cheek (Figure 1) and alteration of the CT and MRI find an expansive tumor process centered on the nasal cavity and maxillary sinus right of 103x 58 x41 vs 156x67x95mm with currently highly elevated spans, the process is globally hypodense and weakly elevated, presence of some vessels as well as hypervascular portions of peripheral localization at the extended jugal level and in front of the internal canthus, bone palace lysis, with a negative extension balance (Figure 2).
Figure 1.Clinical presentation of the patient objectifying the nasal and palatal jugal involvement.
Figure 2.CT scan with PC injection (A) and MRI in axial sections (B) showing the lesion of the right maxillary sinus extended to neighboring structures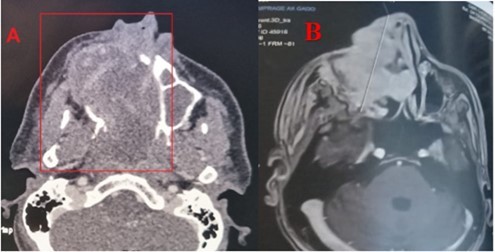
It was removed by an external excision (Figure 3). Histological examination including immunohistochemical staining was in favor of an angiosarcoma NOS (CKAE1, P63: negative). CD31 positive, CD34 negative, factors VIII negative, Melan A negative, UMB45 negative. VIM intense. PS100 focal expression, ERG positive), the resection margins were positive . After the PCR meeting, chemotherapy was decided (Ifosfamide, adriamycin) after two cycles, the patient returned with recurrence of mass with cutaneous jugular extension and orbital a treatment based on propranolol at a dose of 140 mg/ d was initiated with a beginning of reduction in tumor volume after 2 weeks of treatment. Unfortunately the patient succumbed to the disease.
Discussion
Angiosarcoma is a very rare malignant tumour that accounts for about 1 to 2% of all sarcomas 1. Nasosinusial localization is exceptional: 4% of angiosarcomas occur in the pharynx, oral cavity or sinuses 8; only 24 cases have been reported from 1974 to 2009 9. The age range varied between 8 and 81 years, our patient was 40 years old, with a male predominance (16 men for 8women in the 24 cases reported), which was the case with our patient 10. The etiopathogenesis of angiosarcomas is not known, radiation exposure presents a risk up to seven times greater for secondary angiosarcoma 9, vinyl chloride, arsenic and thorium dioxide, which could cause lymphedema, would cause angiosarcoma 11 in our patient, where there was secondary sarcomatous transformation after irradiation. The clinical presentation of angiosarcoma is generally mild in the initial phase 6. The macroscopic aspect is unspecific 12. It comes in the form of polyps or red or purplish plaques sometimes taking the appearance of a hematoma. This misleading clinical aspect requires follow-up and biopsy at the slightest doubt. Our patient had unilateral nasal obstruction with epistaxis of small abundances and smooth reddish mass in the nasal cavity and, at a later stage, the tumor syndrome becomes evident (epistaxis of great abundance, blocked nose, alteration of the general condition) with extension to surrounding structures (eyeball, palate, skin). The radiological presentation is extremely variable and not very specific. On imaging, the tumour has variable dimensions (ranging from 2 to 8 cm in published cases) with hypervascular lesion, heterogeneous contrast uptake and signs of bone lysis on CT scan, and can be evaluated for its extent. In MRI, the tumour has a low-intensity signal on T1 weighted sequences and a high-intensity heterogeneous signal on T2-weighted sequences with an enhancement of intense and heterogeneous contrast 4. The diagnosis of certainty is established by histopathological staining and confirmed by immunohistochemistry 1, 3. Three microscopic aspects have been described: fusiform cells of the epithelioid type and of the undifferentiated or solid type. In undifferentiated forms, the vascular marker CD31 is useful for diagnosis. Other less specific or sensitive markers may be used (Willebrand factor, CD34, lectins) 9. Epithelioid forms pose the problem of differential diagnosis with poorly differentiated squamous cell carcinomas, especially since there is a strong expression of AE1/AE3 cytokeratins in angiosarcoma. In the present case, fusiform cells with CD31 positive vascular markers were found to support the diagnosis of fusiform angiosarcoma NOS 13. Differential diagnosis includes hemangioma, intravascular papillary endothelial hyperplasia (Masson disease), juvenile nasopharyngeal angiofibroma, hemangiopericytoma, Kaposi sarcoma and malignant melanoma 14. The prognosis of these tumours remains bleak today. At five years, there are between 30 and 45% survivors in the localized stage 15. The main prognostic factors are a pejorative size greater than five centimeters; in our patient, the mass has reached 10 cm, a high histological grade, an age greater than 70 years. Resectability, non-RO surgery, and absence of multimodal treatment 16. The treatment is based on surgery (adapted to tumor location and extension) followed by radiation therapy. Other treatment modalities have been tried, such as chemotherapy, radiosurgery (gamma knife) 11, and interleukins 17; and trials with propranolol are currently underway 18. However, no standardized therapeutic management has been defined given the limited number of published cases and the absence of comparative studies. Five-year survival is 22% (versus 12% for soft tissue angiosarcoma in the head and neck) and depends on the degree of tumor differentiation and stage at diagnosis 19. Distant metastases may occur in 30% of cases within the first 24 months; metastases involve bones, lungs, liver, skin or cervix 10.
Conclusion
Radio-induced angiosarcoma is a rare malignant tumour, it occurs in patients who have benefited from conservative treatment and radiation therapy for nasosinusitis cancers. Although major advances have been made in diagnostic modalities such as radiology and histology, angiosarcomas of the nasal passages remain a diagnostic challenge due to their tendencies towards local invasion and distant metastases. Further research is needed to optimize therapeutic approaches to increase long-term survival of patients with nasal angiosarcoma including propranolol which is being studied.
Financial interests
The authors declare they have no financial interests. The authors have no financial or proprietary interests in any material discussed in this article.
References
- 1.Salomons N B, Stearns député. (1990) Hémangiosarcome de l'antre maxillaire. , J Laryng Autol 104-831.
- 2.Gore M R. (2018) Traitement, résultats et données démographiques dans le sarcome sinonasal : une revue systématique de la littérature. BMC Ear Nose Throat Disord. 18, 4-10.
- 3.Chai C, Feng X, Li K. (2023) Angiosarcome des sinus paranasaux avec paralysie faciale comme nouvelle manifestation :rapport de cas et revue de la littérature. BMC Neurol. 23, 428-10.
- 4.Nelson B L, Thompson L D. (2007) Angiosarcome des voies sinonasales : étude clinicopathologique et immunophénotypique de 10 cas avec revue de la littérature. Head Neck Pathol. 1, 1-12.
- 5.Kimura A, Yasuda M, Okamoto S, Tsujikawa T, Hirano S. (2024) Angiosarcome provenant de la cavité nasale : à propos d'un cas. Acta Otolaryngol Case Rep. 31, 41-6.
- 6.Kharkar V, Jadhav P, Thakkar V, Mahajan S. (2012) Khopkar U : Angiosarcome cutané primaire du nez. , Indien J Dermatol Venereol Leprol 78-496.
- 7.Patel V B. (2012) Speer TW : Traitement réussi d'un angiosarcome du nez par radiothérapie. Case Rep Oncol. 5, 570-5.
- 8.Arribas-Garcia I, Domínguez M F, Alcalá-Galiano A, García A F, Valls J C et al. (2008) Oral primary angiosarcoma of the lower lip mucosa: report of a case in a 15-year-old boy.Head Neck. 30, 1384-8.
- 9.Brenda L, Nelson Æ, Lester D. (2007) Angiosarcome des voies naso-sinusiennes : étude clinicopathologique et immunophénotypique de 10 cas avec revue de la littérature.
- 10.Treviño-Gonzalez J L, Santos-Lartigue R, Gonzalez-Andrade B. (2009) Angiosarcome de la cavité nasale : à propos d'un cas. Cas J. 2-1.
- 11.Fukushima Kazuto, Dejima Kenji, Koike Shinobu. (2006) Un cas d'angiosarcome de la cavité nasale traité avec succès par l'interleukine-2 recombinante. Oto-rhinolaryngologie,chirurgie de la tête et du cou. 134-886.
- 13.Agaimy A, Kirsche H, Semrau S, Iro H. (2012) Hartmann ACytokeratin-positive epithelioid angiosarcoma presenting in the tonsil: a diagnostic challenge. Hum Pathol. 43, 1142-7.
- 14.L Di Tommaso, Colombo G, Miceli S. (2007) Angiosarcome des fosses nasales. Rapport d'un cas et revue de la littérature. Pathologica. 99-3.
- 15.Guadagnolo B A, Zagars G K, Araujo D, Ravi V, Shellenberger T D et al. (2011) Outcomes after definitive treatment for cutaneous angiosarcoma of the face and scalp. Head Neck. mai. 33(5), 6617.
- 16.Namyslowski G, Scierski W, Turecka L. (2005) Un cas très rare d'angiosarcome de bas grade des sinus nasaux et paranasaux. Oto-rhino-laryng Pol. 59(1), 105-8.
- 17.Yokoawa M, Tanaka S, Niwa H. (2011) Angiosarcome du sinus maxillaire : à propos d'un cas. Oncologie orale. 47-74.

